Measuring Success
Protecting Millions of People from Disease
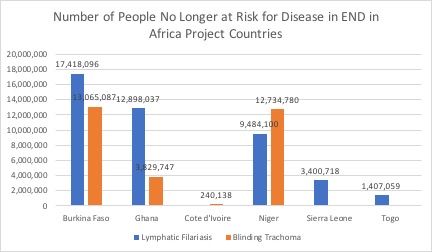
The best measure of the END in Africa project’s impact is the number of people previously at high risk of lymphatic filariasis (i.e., elephantiasis), which causes gross swelling of various body parts, or of slowly going blind from painful trachoma, who are no longer at risk. The chart below shows the number of people no longer at risk for these two diseases in each END in Africa project country. As of the end of FY 2017, a total of 44,608,010 people are no longer at risk for lymphatic filariasis and 29,869,752 people are no longer at risk for blinding trachoma across all six END in Africa project countries.
Districts That Have Reached Stop-Treatment Thresholds
END in Africa’s ultimate goal is to get to the point where lymphatic filariasis, blinding trachoma, and onchocerciasis prevalence is so low that drug treatments are no longer necessary in every health district in all six countries. Once districts reach minimum disease prevalence thresholds, which are set by the WHO for each NTD, countries can stop mass drug administration (MDA) treatments. The number of districts no longer administering treatments is a good measure of the END in Africa project’s impact because every person living in those districts is no longer at risk for disease.
Achievements as of FY 2017
55.9%* of LF-endemic districts have been able to stop MDAs for LF in Burkina Faso, Ghana, Cote d’Ivoire, Niger, Sierra Leone and Togo.
*165 out of 295 districts
69.8%** of trachoma-endemic districts have been able to stop MDAs for trachoma in Burkina Faso, Ghana, Cote d’Ivoire, Niger, Sierra Leone and Togo.
**90 out of 129 districts
As of the end of FY2017, END in Africa countries reported meeting the criteria to stop MDA as follows:
- In Burkina Faso, 55 health districts (HD) have met the criteria to stop MDA treatments for LF, out of 70 HD that were initially endemic. In the case of trachoma, 29 out of 48 originally endemic districts have stopped treatments.
- In Ghana, 83 out of 98 endemic health districts have stopped MDA for LF, and all 37 trachoma-endemic districts have stopped treatment for trachoma continue to report prevalence rates below 5%. Ghana has submitted its final dossier to WHO for the verification of elimination of trachoma as a public health problem.
- In Cote d’Ivoire, 1 of 9 endemic health districts have stopped MDA for trachoma.
- In 2017, Togo became the first sub-Saharan African country to eliminate LF as a public health problem. Trachoma is not a public health problem in Togo.
- In Niger, 11 of 31 endemic health districts stopped MDA for LF and 23 of 35 districts stopped treating for trachoma.
- In Sierra Leone, 8 of 14 endemic health districts stopped MDA for LF. Trachoma is not a public health problem in Sierra Leone.
Assessing the Treatment Impact
According to the World Health Organization, many neglected tropical diseases (NTD)—including the seven that are the focus of END in Africa’s efforts–can be successfully eliminated after six years of mass drug administration treatments in endemic regions. As the END in Africa countries get closer to disease elimination, they will begin to shift their efforts from mass drug administration to treatment evaluation and monitoring for disease cases.
In the second half of FY 2017, the following disease surveillance activities (DSA) were conducted through END in Africa:
Assessments conducted in Q 3–4, FY2017, by country, type of assessment and disease*
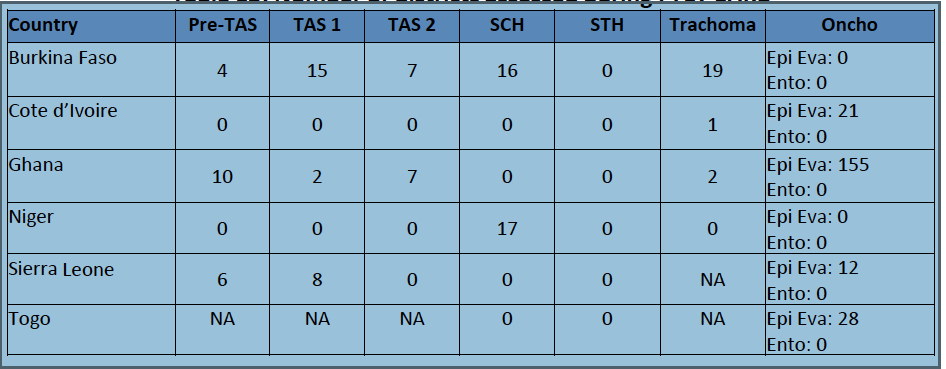
* Epi Eva: Epidemiological evaluation; Ento: Entomological; Pre-TAS: Pre-transmission assessment survey; TAS1:Transmission assessment survey conducted several years MDA has been stopped; TAS2: TAS conducted five years after MDA has been stopped.
A survey is a survey is a survey?
How countries measure progress towards disease elimination: An overview of disease transmission surveys and assessments
Deciding when to stop MDA interventions in a community, region or district can be tricky. Stop MDA too soon and NTDs can regain their foothold and re-infect populations that were thought to be disease-free. Keep MDA going too long and valuable time, energy and resources are wasted.
To complicate matters further, transmission assessment is done a little differently for each NTD. So, it’s not surprising that NTD country programs and their partners, including END in Africa, put substantial time and effort into monitoring and evaluating the impact of their MDA interventions.
The various disease transmission instruments used to evaluate the impact of MDA interventions for each NTD addressed by END in Africa are summarized below.
A transmission assessment survey measures whether each countries’ pre-determined evaluation units (i.e. districts) have lowered the prevalence of infection to a level where disease recurrence is unlikely, even after MDA interventions have stopped. In the case of lymphatic filariasis (LF), current WHO guidelines recommend that countries conduct a formal Transmission Assessment Survey (TAS) to determine whether MDA can be stopped in an area that has had at least five rounds of annual MDA.
Prior to doing a formal TAS, END in Africa countries typically monitor the effectiveness of MDA interventions through so-called “Pre-TAS” surveys, including spot checks and sentinel site surveys. Both sentinel site surveys and spot checks collect data on parasitological data to measure disease prevalence in pre-determined geographical areas. However, the geographical locations of sentinel sites do not change over the course of the program, while spot checks may be done at different locations each time. In the case of LF, districts with parasite prevalence below 1% of the group surveyed are considered “non-endemic.”
The WHO has produced a table outlining disease-specific guidelines for the neglected tropical diseases addressed by END in Africa.
Number of people no longer at high risk for LF*
44.6 Million
*FY 2017 data
Number of people no longer at high risk for blinding trachoma*
29.8 Million
*FY 2017 data

Photo Credit: FHI 360