Cross-Border Collaboration: Synchronizing Treatment for NTDs in West Africa
February 28th, 2017
After six years, during which over 429 million treatments were administered to over 202 million people, many of the six END in Africa-supported countries are ‘walking the final mile’ in the fight against several neglected tropical diseases (NTDs)—namely elephantiasis and trachoma—with plans to stop nationwide mass drug administration (MDA) for these two diseases by 2020. As their capacity to manage integrated NTD programs has improved, these countries have succeeded in maintaining good treatment coverage and in gradually reducing NTD prevalence. However, their achievements may be at risk if the diseases are ever reintroduced into the countries, such as through migration from countries that have not yet controlled these diseases.
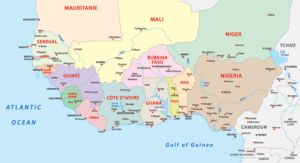
Resurgence, recrudescence, or importation of NTDs (especially elephantiasis and river blindness) from neighboring endemic countries is an ongoing concern in Africa. Evidence shows that the black fly—the insect that carries the river blindness-causing microorganism from person to person—can travel up to 400 km with the wind.[i] In addition, borders in West Africa are poorly monitored, despite continuous migratory flows. Thus, it’s hardly surprising that cases have been reported of cross-border disease transmission of NTDs such as elephantiasis.[ii] The recent outbreak of the Ebola Virus Disease (EVD) in 3 West African countries (Guinea, Liberia and Sierra Leone) is a case in point of how easily infections can spread across borders.
Given this phenomenon and the fact that progress toward NTD control varies from one country to the next, national health authorities need to know what their countries can do to prevent cross-border transmission of NTDs. Experts believe that improving inter-country cross-border collaboration and synchronizing MDA in border districts can prevent cross-border NTD transmission. Although many African countries already participate in various cross-border collaboration platforms that meet regularly to share information on NTD control, learn from each other’s experiences, and sometimes provide technical support to each other, lack of follow-through in the implementation of meeting recommendations has been a problem, especially in regard to synchronizing mass treatment in border districts. Countries have found it difficult to conduct synchronized treatment because they often work with different organizations for support on NTD control and funds for NTD control are often provided at different times of the year in different countries.
Enabling Synchronized MDA: Strategy in END in Africa-Supported Countries
Four of the six END in Africa-supported countries share common borders: Burkina Faso, Cote d’Ivoire, Ghana, and Togo. On October 27, 2016, FHI 360 organized a meeting in Accra, Ghana, to promote cross-border collaboration, bringing together representatives of these four countries with the goal of translating ‘talk’ into ‘action.’ In this meeting, the representatives focused on developing strategies to implement the recommendations of World Health Organization (WHO) Regional Committee Resolution AFR/RC57/R3 of 2007, which seeks to intensify cross-border activities, strengthen surveillance, and thus, avoid transmission of infectious diseases to areas that are considered “disease-free,” The countries used the meeting to identify priority districts, agree upon a timeframe, and anticipate challenges that would need to be addressed to successfully synchronize MDA.
The following conclusions emerged from the October 2016 meeting:
- Although MDA for river blindness is expected to continue beyond 2020 in the END in Africa countries, synchronization of MDA for river blindness and elephantiasis will be required in selected border districts as a prerequisite for disbursement of END in Africa-managed funds for conducting MDA in those districts. Exceptions will be made if countries demonstrate that synchronization is not possible.
- International coordination among USAID’s NTD program, the END in Africa project, and other partners that work with the four national NTD programs, will be required to respond to problems that may impede the planned synchronization.
- The END in Africa project will appoint a liaison officer to facilitate coordination among USAID, FHI 360 and the countries, to ensure that the countries receive medicines each year before May (i.e. early enough to successfully implement planned MDA). The liaison officer will work with the countries to ensure that drug request packages are submitted on time. In the case of delays, USAID and FHI 360 will contact WHO to resolve the situation.
In order to further support the synchronization of MDA along border districts in FY 2017, the conclusions reached at the meeting now form the basis of contractual agreements between the countries and the END in Africa project. The experience gained from this pilot project will be shared to motivate other organizations to form similar agreements in countries they support with shared borders.
[i] Crump A et al. (2012). The onchocerciasis chronicle: from the beginning to the end? Trends in Parasitology; 28(7): 280-288.
[ii] Ramaiah KD (2013) Population Migration: Implications for Lymphatic Filariasis Elimination Programmes. PLoS Negl Trop Dis 7(3): e2079. doi:10.1371/journal.pntd.0002079; Bhumiratana A et al. (2013a) Border malaria associated with multidrug resistance on Thailand‐Myanmar and Thailand-Cambodia borders: transmission dynamic, vulnerability, and surveillance. Biomed Res Int 2013:363417; Bhumiratana A et al. (2013b) Current Bancroftian Filariasis Elimination on Thailand-Myanmar Border: Public Health Challenges toward Postgenomic MDA Evaluation. ISRN Trop Med 2013: 857935.